
The Vaping Debate Heats Up: Key Insights from the E-Cigarette Summit 2023
Vaping is at a crucial juncture, with the UK government considering banning flavours, imposing vape taxes, enforcing plain packaging and other measures.
At this key time, the superb E-Cigarette Summit has once again brought together top experts and scientists for an unparalleled exchange of science, evidence and (often conflicting) views.
The themes and questions this year are powerful. They include:
- How misinformation is spread by the media, some tobacco control groups and even the WHO is keeping smokers smoking, leading to devastating death and disease.
- How focus has increasingly shifted from smoking to vaping - with severe consequences.
- How do we encourage smokers to switch to vaping - and at the same time discourage young people from vaping, without inadvertently nudging them towards smoking?
- How different vaping policies in different countries have impacted smoking and vaping rates - with results varying from almost eliminating smoking to increased youth smoking and a thriving vape black market.
Here you’ll find some of the key data, arguments and points recorded by me and my colleague Kayleigh. As always, it’s impossible to capture all the rich detail, or even all the presentations, so do watch the videos when they are available - and, if you are able to, make sure you sign up to next year’s summit.
Contents
- Session 1: Science & Evidence
- Session 2: Policy & Research
- Session 3: THR, Nicotine & Public Health
- Session 4: Tobacco Control & Regulation
- Have your say
- Related guides
Session 1: Science & Evidence
Opening Keynote: Are we scapegoating young people and where should collective responsibility lie?
Prof Caitlin Notley, Chair of Addiction Sciences - University of East Anglia
By Kayleigh
With vape horror stories in the news and talk of a “child vaping epidemic”, Prof Notley wants the voices of young people themselves at the forefront of our thinking on the subject.
Why do they vape? Peer influence is a prominent theme - with vaping seeming ‘trendy’ or ‘cool’ and something they undertook as part of their social group. But there’s also stress and anxiety management, along with vaping becoming normalised behaviour “like using a mobile phone”.
More concerning behaviours included use of black market ‘9000 puff’ devices, and dangerously tampering with disposable batteries to make them last longer.
With taxes on vapes looming, it’s worrying that some kids think it is cheaper to smoke than vape.
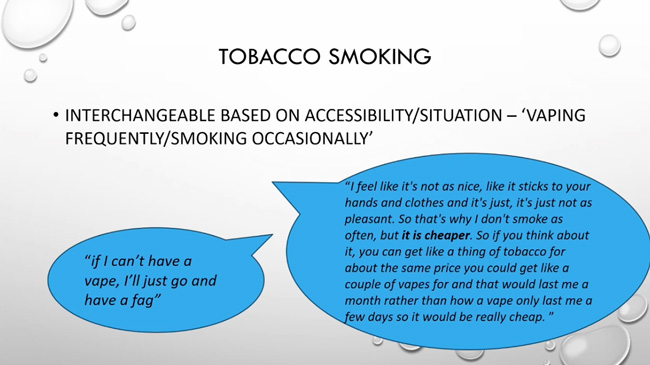
Cost and availability is not the only reason children switch between smoking and vaping.
Kids are worried that vaping can lead to:
- coughing up blood
- lungs getting ‘fried’
- popcorn lung
In fact, some think vaping is worse than smoking.
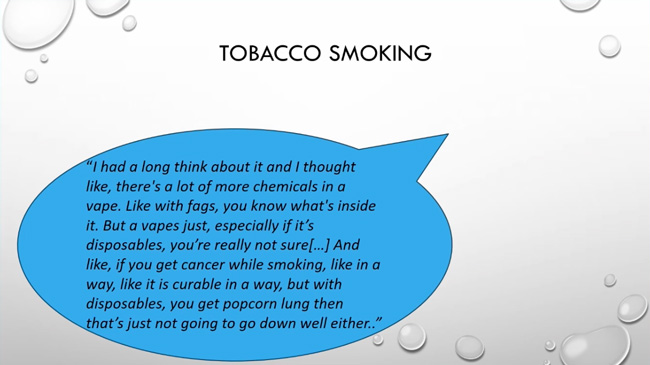
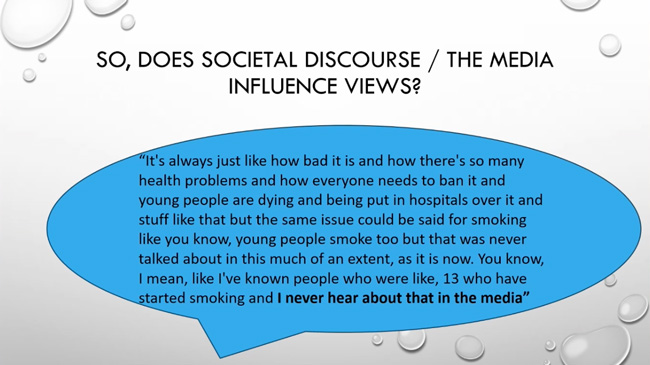
Why? Media horror stories - and the switch in focus from smoking to vaping.
In the end, we all need to stop scapegoating young people and take responsibility for the situation we find ourselves in.
Regulators have been too slow to catch up to the proliferation of products and the way they are marketed, parents and researchers also need to take responsibility to tackle the issue and the media needs to be responsible for the incorrect messages they are relaying to young people.
Complex problems, clumsy solutions and the court of public opinion
Prof Sanjay Agrawal, Professor of Respiratory Science, Institute of Lung Health - University Hospitals of Leicester NHS Trust, Special Advisor on Tobacco, Royal College of Physicians
By James
Professor Sanjay opened up with some history - including early attempts by King James to restrict nicotine use through a 4000% increase in tax. I always like these historical comparisons, as they put current tobacco control attempts into context.
There were two key points here.
First is poor media coverage that is leading the public to believe that vaping is as bad or worse than smoking.
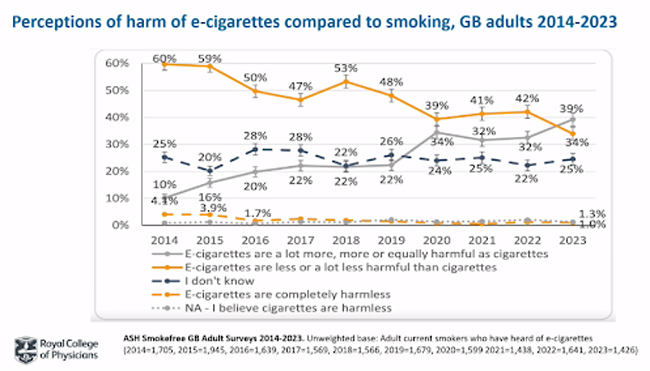
The massive problem here, the death, disease and devastation caused by tobacco, is now being ignored by the media in favour of spreading what is often misinformation about vaping. Because of that, people keep smoking.
Secondly, nicotine use and vaping is a complex problem. Agrawal argues the best we can do to tackle complex problems is with what he calls ‘clumsy solutions’, applying imperfect but responsive measures to be monitored and adjusted over time.
Is vaping an effective and safe aid for quitting smoking? The Cochrane review of electronic cigarettes for smoking cessation
Prof Peter Hajek, Director of the Health and Lifestyle Research Unit - Wolfson Institute of Population Health, Queen Mary University of London
By Kayleigh
The Cochrane review determines the usefulness of treatments - providing evidence for policymakers to make informed decisions. Prof Hajek emphasises the use of meta-analysis - a statistical method involving the combination of multiple randomised trials.
Can e-cigarettes help people stop smoking? Yes, there is now substantial evidence, including 47 randomised trials (7 in the last year) as well as non-randomised studies and cohort studies.
Studies focused on 3 key comparisons and measured quitting over 6 months
- E-cigarettes vs nicotine replacement treatment (NRT)
- E-cigarettes vs non-nicotine e-cigarettes
- E-cigarettes vs no treatment/just advice
The most important of these is the comparison between e-cigarettes vs NRT, as NRT is one of the oldest, most established methods for quitting smoking. Smokers are 60% more likely to quit with e-cigarettes than with NRT. This was given a high certainty of evidence grade, with a solid verdict that is doubtful to be contradicted by new evidence.
This shows e-cigarettes are effective as a smoking cessation tool, with studies showing no clear evidence of major harm in up to 2 years of use.
Practically, this, combined with other major studies, means health professionals can conclude that YES, e-cigarettes can help with quitting smoking and, while long-term there may be risks, these are only going to be a fraction of those from cigarette smoking.
The strategic vision for ending smoking in the UK and future policy discussions
Prof John Newton, OBE FRCP FFPH FRSPH, Director of Public Health Analysis - Office for Health Improvement and Disparities (OHID)
By James
Smoke free by 2030. That’s the government’s goal, but modelling suggests that we’re not going to achieve it. That’s a problem because smoking is still killing a huge amount of people - more than the entire amount killed by the pandemic every 2-3 years.
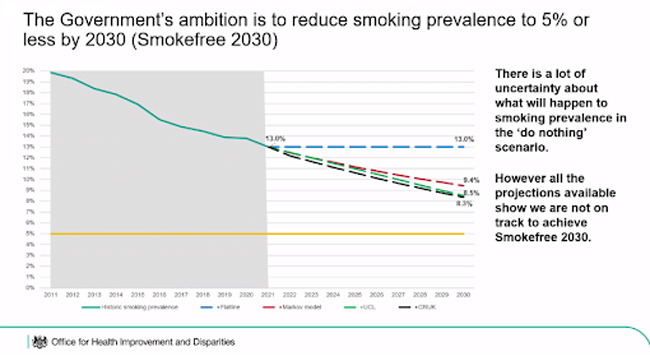
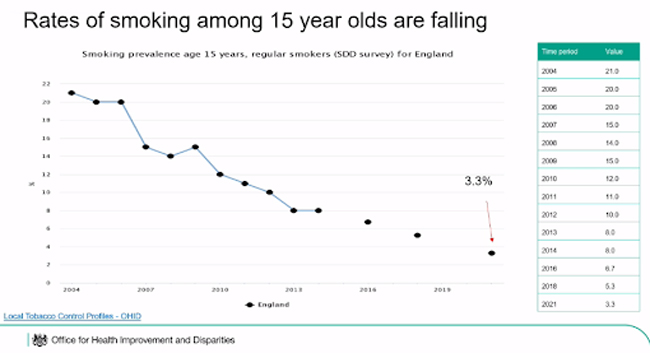
Overall smoking is coming down, particularly in younger groups like 15 years olds. but it’s getting worse in other groups, and it’s also increasing inequality.
Electronic cigarettes can play a big role in achieving this goal - and as their use has increased, smoking rates have fallen. At the same time, it’s concerning that 1.1% of non-smokers now vape.
We know vaping is much less harmful than smoking, and that it helps people stop smoking. We also need to overcome the perception that vaping is as bad or worse than smoking. However, we don’t want people who don’t use nicotine to start vaping.
How to solve this with policy? There’s no single intervention. You might say we can ban disposables and that will solve the issue, but as Caitlin’s presentation demonstrated, it’s more complex than that.
We need legislation, we need enforcement and we need money to support public health campaigns and the multiple organisations working to tackle smoking. It’s also important to have partnerships to crack down on illegal trade.
Session 2: Policy & Research
Disposable vapes in Great Britain: Impact and implications
Dr Harry Tattan-Birch, Research Fellow - University College London (UCL)
By James
Dr Tattan-Birch used data from The Smoking Toolkit study to explore the increase in disposable vape use.
Disposable vape use is rising fast, especially in the 18-24 age group. While smoking rates are falling, they are not decreasing as fast as disposable use is increasing. That means that, overall, inhaled nicotine use is increasing. What’s more, smoking rates are falling at the same rates as pre-disposable use, although there is a slight rise in older groups, so vaping could be offsetting this rise.
What to do? We could ban disposables, but this could lead to a number of pitfalls. 750,000 smokers have switched to disposables, and these people could go back to smoking. What’s more, the industry could find loopholes (such as putting a USB charging port in disposable devices) and, as has happened in other countries, the black market could take up the slack.
Two options he discussed include:
Putting a tax on disposable vapes: Tartan-Birch seems to think this is an option. I really don’t understand how you can acknowledge the black market is a problem and then suggest a tax. Who would buy a legal disposable for £10.00 when you could buy illegal disposables for less than half the price? Let’s not forget that Notley’s study found that kids are already talking about smoking being cheaper than vaping, while Friedman’s talk showed that vape taxes increase smoking rates.
Packaging/displays: Another option is to remove all the colour from products and/or put them behind the counter or in a locked box. I think this would aid the black market - and, as other talks highlight, it would be a great way to reinforce the perception that vaping is as bad or worse than smoking!
Harry also discussed restrictions on advertising, which is currently allowed on buses, billboards and the internet, and on flavours, which he acknowledged could have a catastrophic effect as most ex-smoking vapers use non-tobacco flavours.
I’m disappointed he didn’t mention vape licensing, which could raise money for enforcement, increase the motivation for stores to follow rules and make life easier for Trading Standards while avoiding increasing the cost of vapes for smokers.
Will a change in packaging policy reduce youth e-cigarette use in the UK?
Eve Taylor MSc, PHD Student and Research Assistant - Nicotine Research Group - King's College London (KCL)
By James
Eve has been conducting research to find out how packaging restrictions affect consumers' perceptions of vaping products. She did this by presenting branded and non-branded products to youths and adults and asking them how it would affect their choices.
She found that plain packaging did not decrease the appeal of devices to adult smokers but did decrease the appeal to youth. However, children were more likely to think that vapes and e-liquid in plain packaging were as bad or worse than smoking.
While I wouldn’t offer Eve a job in our marketing department, I’d love to see this relative attraction trialled in real life as, given the plethora of black market products out there, plain-packaged vapes will have to compete with colourful illegal products. It also runs counter to the fact that vape brands with plainer packaging have badly underperformed in recent years.
Risk perceptions of e-cigarettes
Sarah Jackson, Principal Research Fellow Behavioural Science and Health - University College London (UCL)
By James
Public Health England 2015:
In an effort to communicate the relative risk of vaping, the UK has stated that vaping is 95% safer than smoking. The US has concurred vaping is safer than smoking, although they have been reluctant to put a figure on it. 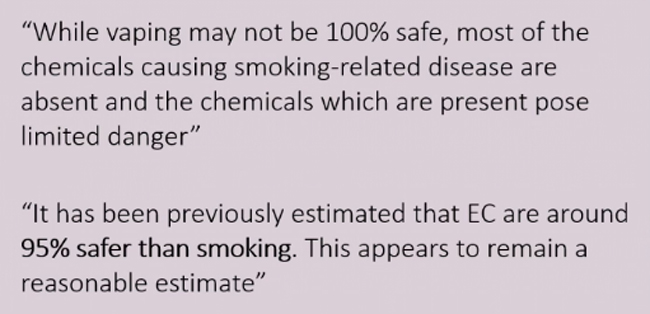
Then we had the lung disease EVALI. The very name (E-cigarette or Vaping Product Use Associated Lung Injury) suggests this is a vaping disease when it is clearly caused by Vitamin-E Acetate in illegal cannabis products. However, this disease had a massive impact on perceptions of vaping safety.
The effort to explain relative safety has been criticised by one prominent researcher (I’m guessing this is Martin McKee), who argues that this has increased vaping rates, although he didn’t actually disagree that vaping is safer than smoking.
In fact, the evidence tells us that, far from accepting the government’s view, due to worldwide misinformation more people think vaping is harmful. The rise in vaping is due to the popularity of disposables, not because people think it is safe. 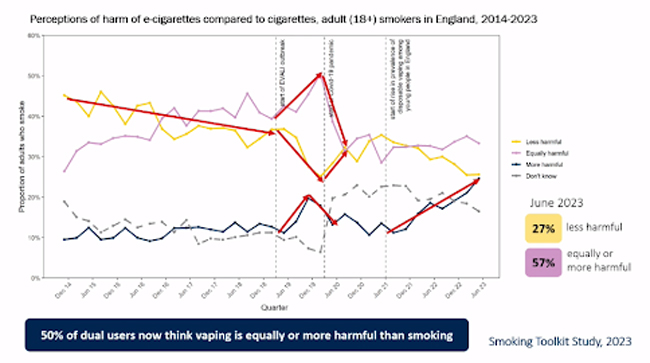
“We're told overwhelmingly that vaping is not safe… that vaping barbecues your lungs, that vapes contain chemicals that can rot your flesh, that your lungs could collapse within weeks of use.”
The perception that vaping is worse than smoking is being reinforced by some medical professionals:
“Just this summer, a paediatric physician at a London hospital warned that if a teenager starts smoking, the worst that will happen is that they'll be sick behind the bike shed, but that vaping could put them in intensive care. Now, of course, there are some more balanced media stories out there, but which are people going to remember?”
People often point out that it took us a long time to know smoking would be bad for us, and that it could be the same for vaping. However, science has moved a long way from then, and:
“...people need to understand that if cigarettes were invented today, we'd know immediately that they're incredibly harmful.”
What are the consequences of misinformation? It could:
- prevent smokers from switching
- lead to continued dual use of vapes and cigarettes
- mean that young people who are inclined to use nicotine might start smoking instead of vaping.
To counter this, we need public health information about vaping and we need to urgently bridge the gap between what the evidence tells us about vaping and what people actually think. One of the best ways to do this is to use experts to debunk common myths.
At the same time, Jackson warned that the measures the government is considering, such as restricting point of sale and restricting the sale of disposable vapes, could increase the public perception that vaping is at least as bad as smoking.
Restricting flavoured e-cigarette sales: Policy effects & alternatives
Assoc Prof Abigail S. Friedman, Department of Health Policy & Management - Yale School of Public Health
By James
When we increase prices on cigarettes and make smoking less attractive, smoking rates go down. However, microeconomics also tells us that when we make the alternative (vaping) more expensive and less attractive, smoking rates go up.
We can see this with flavours, which have been restricted in large parts of the USA. This leads to decreased vaping rates, increased smoking rates and increased smokeless tobacco use. Specifically for every pod not sold because of flavour restrictions, an additional 15 cigarettes are sold.
While some of Friedman’s data is preliminary, she highlighted that any public health benefit of reducing end use by restricting flavours could be offset by public health damages from increased cigarette use.
Harm reduction beyond e-cigarettes: how do heated tobacco products compare?
Prof Lion Shahab, Professor of Health Psychology, University College London - Co-Director of the UCL Tobacco and Alcohol Research Group
By James
Sales of Heat Not Burn (HNB) products have soared in countries where vaping is restricted. Heated tobacco products clearly cause much less harm than cigarettes, but at the same time, they cause more harm than vaping.
HNBs are more expensive and addictive than electronic cigarettes, but at the same time, they may be more satisfying. They also allow people to retain their identity as a smoker. We also have to bear in mind that they may increase long-term nicotine use with an increased risk of relapse to smoking than other options.
In summary, Lion felt that HNBs should have a more limited use in tobacco harm reduction and should be limited to smokers who have tried and failed to quit with other methods.
Why is the MHRA e-cigarette notification scheme essential for the short and long-term protection of public health?
Craig Copland, Head of E-Cigarettes, Healthcare, Quality and Access Group - MHRA - The Medicines and Healthcare products Regulatory Agency
By Kayleigh
Craig discusses the work of the MHRA and the interesting trends seen regarding e-cigarettes, particularly disposables, in the last couple of years - with various changes and unintended consequences.
There has been a huge increase in disposable vape product notifications in the UK in the last couple of years - making up 50% of 32,000 new notifications.
Before this, disposables were already flooding the market - just not legally. But illegal vapes are still a huge problem - with the 75,000+ illicit vape products seized in the first quarter of 2023 being ‘just a drop in the ocean’.
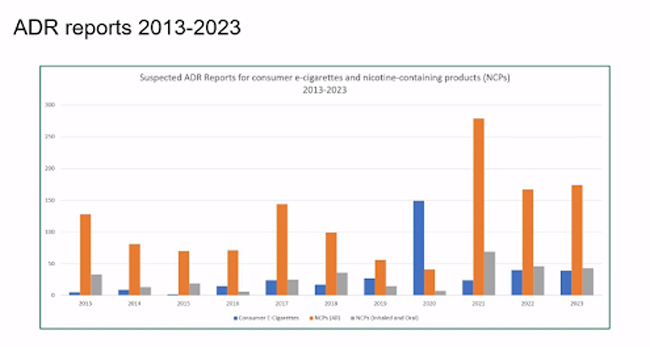
He also covered the Yellow Card Scheme, which is a way to report adverse drug reactions (ADR). Craig argued that it is easy to misinterpret these numbers, and paint a bad picture about vaping in the media, but to give context you need to compare these figures to reports from Nicotine Replacement Therapy (NRT) products.
Note, I was a little confused here as the data showed NCPs (nicotine-containing products )- I assume from the talk that this referred to NRT.
Craig also cited the number of people calling for ‘better enforcement’ when it comes to illicit products, and argued that this is not the case. The work of enforcement agencies is ‘phenomenal’ - but there aren’t enough officers to do what is, after all, only one part of their job. What we need is more officers, better training, better regulation and better policies.
Session 3: THR, Nicotine & Public Health
Swap to Stop – Going for a million
Martin Dockrell, Tobacco Control Programme Lead - Office of Health Improvement & Disparities (OHID)
By James
We need a tenfold increase in quit attempts to reach the Smokefree 2023 target. One way to help achieve this is the Swap to Stop Scheme, an ambitious attempt to give a million vape devices to smokers. These will be done in a number of ways, including partnerships with stop smoking services and via a digital offering.
Enthusiasm has far exceeded Martin’s expectations so far, with applications for a quarter of a million vapes in the first month (bear in mind this is a multi-year scheme). There will also be new training to help stop smoking services from the NCSST (National Centre for Smoking Cessation and Training) from early 2024, and exciting opportunities to reach disadvantaged groups such as the homeless.
Opportunities and dilemmas- how Fresh is addressing vaping within a collective shared vision for a Smokefree Future
By Kayleigh
Ailsa Rutter OBE, Director - Fresh and Balance
Ailsa Rutter is the director of a charity that works to reduce smoking. She seeks a dual approach to vaping. On the one hand, she pointed out that people need multiple options to stop smoking. This requires mass media campaigns to highlight that vaping can help people stop smoking and balanced education on vaping for young people.
On the other hand, she would like to see restrictions on vaping. This includes increasing the prices of vape devices (taxation), hiding them from sight in shops and measures to reduce branding.
Hazel Cheeseman, Deputy Chief Executive & Policy Director - ASH
While there are some inconsistencies in how UK media portrays vaping, most public health organisations are following the lead of the Chief Medical Officer: If you smoke, vaping is safer. If you don’t smoke, don’t vape.
There has been a lot of emphasis and activity around the country on building consensus, having shared-position statements, producing practical advice and taking a comprehensive approach that gives people practical measures to implement.
In terms of youth vaping, there have been worrying reports on how vaping is impacting school environments. The aim is to give young people balanced and accurate information on vaping and to guide schools on how to construct their policies in an appropriate way (rather than panicking!)
The North East is really taking on a policy challenge with e-cigarettes and trying to strike a balance between advocacy for adults to switch and protecting young people.
Finally, while many sessions today have focused on facts, this session was a little different and ended on a real-world note. A video was played representing the real-world effects of smoking - with a cancer sufferer who has now switched to vaping sharing the devastating effects smoking had on her life and that of her family - hitting home the real reasons we need change.
The North East North Cumbria’s approach to vaping and a respiratory clinician’s perspective
Rachel McIlvenna, Smokefree NHS Strategic Manager - North East and North Cumbria ICB
Dr Ruth Sharrock, Clinical Lead for Tobacco Dependency for the North East & North Cumbria ICS - Respiratory Consultant, Queen Elizabeth Hospital - Gateshead
By James
After lots of numbers, graphs and theoretical models Ruth, a typhoon of emotion and passion straight from the cancer and respiratory wards, came in to remind us of the realities of what smoking is doing to people:
She talked to us about people…
“...who have reached an absolute crisis point in their life, the wheels have come off and they've ended up in hospital, they're terrified, they feel out of control about their situation and they have really very little resource to deal with all of that.”
This included people who have been rushed into hospital barely able to breathe, their face shut off with a tightfitting oxygen mask:
“you're utterly trapped, scared, agitated, out of control and for those dependent on tobacco the fear of the experience is just magnified dramatically.”
Vaping helps.
“I can tell them it is vastly safer, it's effective, it's easy, it's literally swapping the cigarette out of their hand for an e-cigarette, easy to use and for many of these people it means that the first thing they do when we finally relieve their hypoxia, they can breathe again, disconnect some things, they don't go outside and breathe in combustible tobacco in the next breath, so it's such an important treatment for them.”
It helps with lung cancer diagnosis too. Quitting smoking can double life expectancy, but it's often too much to cope with on top of everything else. Vaping is a credible, believable offer “that will help them and put them in a position where when they come back for all the results that we can actually offer them some treatment.”
Ruth concluded with a plea; put the needs of the people who need vaping the most at the forefront of any policy.
Swap to Stop: How vaping has become mainstream
Louise Ross, Clinical Consultant, NCSCT - Chair and Mental Health Lead, New Nicotine Alliance
By James
After a number of talks from scientists who approach vaping as a medical solution to a disease, it was a breath of fresh air to hear Louise Ross talk.
Incorrect evidence is still circulating, and this is keeping people smoking. For example, Louise suggested vaping to a woman smoker on a train recently, only for the woman to say: “No, they’ll kill you them things.”
However, vaping has become accepted by key bodies in the UK like Lung Cancer Research and NICE (National Institute for Health and Care Excellence) - a body known for only accepting strict evidence. Using quotes from these bodies can be a shortcut to acceptance of vaping - but when a doctor or consultant tells smokers vaping is bad there is nothing Stop Smoking Services can do.
Louise then backtracked to talk about how the acceptance of vaping came about in the stop smoking community. For many people, using vaping as a tool to help smokers was a risky move that could have killed their careers. At the time, we didn’t have the body of evidence we do now, and it took open mindedness and a gut feeling to embrace vaping.
Louise also covered the issue of disposables, particularly with people who go straight to vaping without smoking first.
“I'll ask some of you, how long should they smoke before they switch? Should they start smoking and smoke for a month and then switch? A year? … Is that a sensible choice?”
She criticised stop smoking practitioners who told people that vaping was a 12 week course. This was not sensible, and showed a desire to have control over the service users and the treatment program.
Perhaps controversially, Louise tackled the argument that vaping is worse than breathing fresh air. She compared and questioned the attitudes between drinking alcohol and vaping, asking why it was okay to drink alcohol and not to vape.
Session 4: Tobacco Control & Regulation
E-cigarettes and tobacco control in Great Britain: Where are we now and why?
Deborah Arnott, Chief Executive - Action on Smoking and Health
By James
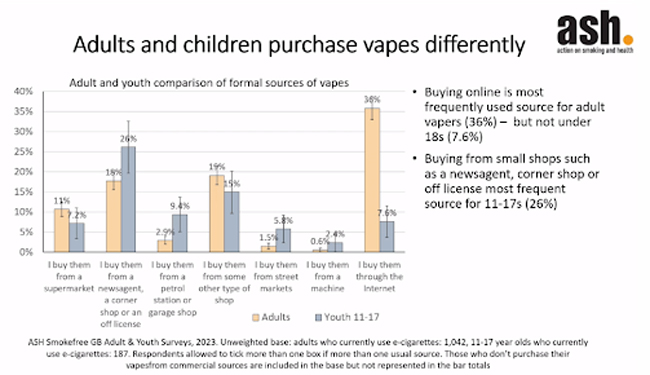
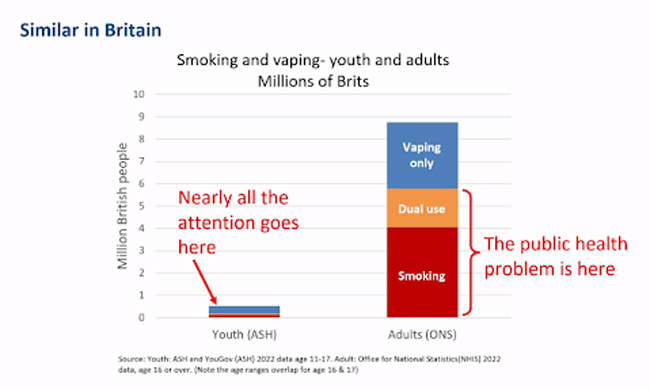
Deborah started off by highlighting that there are 4.7 million adult vapers, most of whom are vaping either to quit smoking or to prevent relapse. There are lots of dual users, but we understand now that this is a step on the way to quitting smoking. There are 400,000 underage vapers, of whom a quarter hadn’t previously smoked, with a rough split of 50:50 between regular and occasional use. 
Where are kids getting vapes from? Mostly not online, but instead from shops like newsagents and off licences. There’s lots of overlap between flavours between adults and children, but children are more likely to prefer candy flavours. The main reasons for kids trying it is experimentation and peer pressure.
Then, in front of a room full of scientists who had been emphasising the danger of misperceptions due to individual reports of harm amplified by the media she talked about a non-smoking friend who tried vaping and then had to have a filling for the first time.
This is a clear example of taking a single data point amongst millions and then trying to make a point with it. I’ve personally been vaping for 15 years, and have never had a filling, and using the same rationale I would be able to argue that vaping is good for your teeth.
Neither are valid arguments, and when we have solid studies on vaping (including ongoing research into the relationship between vaping and dental health) we don’t need people who influence policy to start using anecdotes to make health points.
Deborah then went on to argue for taxation on vapes, arguing that illegal tobacco had been dealt with in the UK [note, according to the ONS, lost tobacco tax revenue has fallen from GBP 2.5 to 2.3 billion and the illicit market is now 16% of total sales] and if vapes were brought under taxation the same would be the case of vapes. The revenue raised could then be used for enforcement. Apart from specialist vape shops, products should be put behind a counter and promotions should be banned.
The smoking endgame and youth vaping in New Zealand
Ben Youdan, Director - ASH New Zealand
By Kayleigh
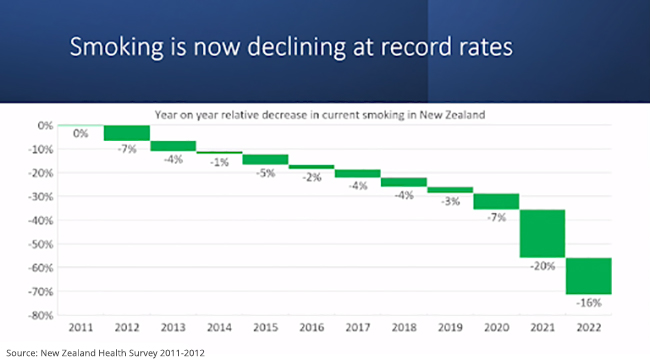
Ben Youdan’s presentation is particularly interesting, as it shows what can happen when stop smoking policies are combined with vaping uptake.
In New Zealand, consumers can buy vape products at up to 5% nicotine strength. While flavours are severely limited in general stores they are completely unrestricted in specialist vape stores.
New Zealand’s smoking endgame is in sight- a continuously declining smoking rate and a record low of 8% currently smoking daily. Vaping has had a profound effect on this, with this - with a strong correlation between falling smoking rates and an increase in vaping. There has been a 40% decrease in smoking in the past 4 years alone - something which had previously taken a decade to achieve.
Around 60% of daily vapers in New Zealand are former smokers and, while 10 -12% are ‘never smokers’, just 3% of these report having never actually smoked a cigarette before.
Ben feels other countries need to look at and copy New Zealand’s policies, while remembering that embracing vaping has given the NZ government confidence to pursue aggressive anti-smoking measures such as mandating low-nicotine cigarettes and introducing a smoke-free generation policy.
However, with the smoking end-game on the horizon, the focus has now shifted to vaping as a perceived public health problem - with the main arguments being the harms of nicotine addiction and the effects on young people. It’s true that vaping numbers have increased, but this pattern has reversed since vaping legislation was introduced. 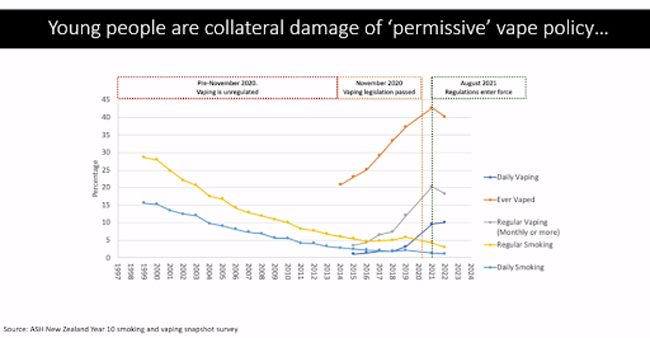
Ben feels using language such as ‘generation of nicotine addicts’ is incredibly harmful and portrays nicotine users as helpless victims - diminishing their voice and agency. He also argued that the attitude to young vapers is causing more harm than vaping:
“We've had a 450% increase in young people being suspended or expelled from school because of vaping, with a health NGO saying, vaping is causing harm, it's robbing people of their futures because they're being suspended and expelled from school for vaping."
Well, the harm here is the response, it's not the vaping. And we're doing things to young people who are vaping, which is more harmful from the behaviour that we're trying to stop itself.
Why are kids vaping? The New Zealand government asked children and:
“...for a lot of it, it's just a phase, we're just trying it. We use vaping as a coping mechanism when we're stressed or we're anxious.”
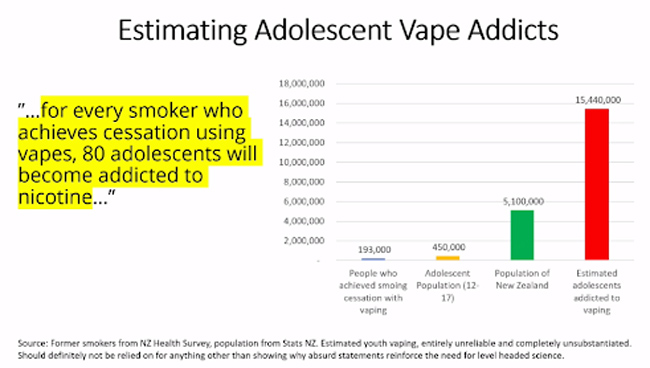
Misinformation is another issue - with a recent press release from a New Zealand NGO claiming that for every smoker who quits via vaping, 80 adolescents become addicted to nicotine. Ben’s calculated that this would result in 15.5 million nicotine-addicted youth - 3 times the actual population of the country!
Meanwhile, in Australia, laws have effectively government-sanctioned a monopoly on the most harmful form of nicotine by restricting vaping whilst leaving cigarettes on sale. The results?
- An increase in the number of vapers.
- 9 in 10 vapers use illegal, potentially dangerous devices.
- Stagnation on smoking rates, with Australia now overtaken by the UK, the USA and New Zealand.
- An increase in youth vaping rates.
- An increase in youth smoking rates.
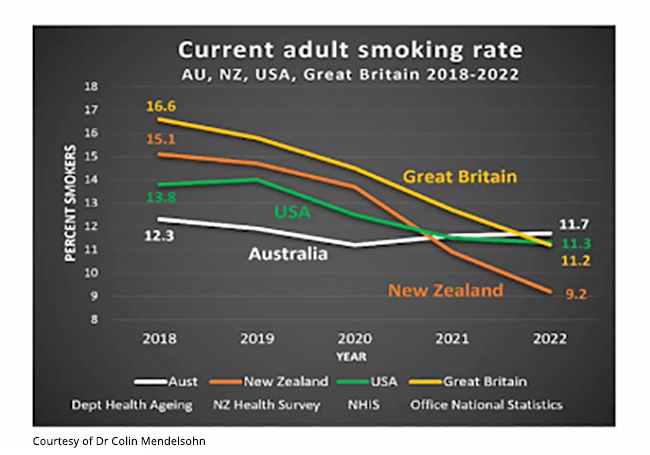
Yet, despite this, Australia continues to double down on its measures rather than looking at the success of the UK and New Zealand.
Ben concludes with a quote from a book by Maja Sazlovic:
"Stopping an evil drug from theoretically corrupting children mattered more than the lives of the people who are already using it."
The same, Ben says, applies to nicotine.
Tobacco harm reduction in Southeast Asia - challenges and opportunities
Prof Tikki Pang, Former Director, Research, Policy & Cooperation, World Health Organization - Geneva, Switzerland
By James
I wanted to cover Tikki’s presentation briefly because it highlights that while we’ve made a lot of progress on smoking in the UK, that progress is not being reflected in the rest of the world.
In the ASEAN region alone, 127 million people smoke, with more than half a million dying each year from tobacco-related diseases.
Why?
In most of the region, there’s huge opposition to vaping, with the safer alternative banned in many places where smoking remains legal. There’s a lack of leadership - and there’s also the hostile position of the WHO (which as other talks pointed out has spread misinformation and lies about vaping). Finally, there is:
“...polarised, acrimonious, and unproductive dialogue… fueled, surprise, surprise, by misinformation and disinformation and biassed selective use of evidence, cherry-picking, if you like.”
The key to the problem is a disconnect between the harm reduction community, which wants to eliminate smoking, and those who want a nicotine-free society.
There is hope. One lies in the potential for leadership change at the WHO, and another in the leadership set by countries like New Zealand and the UK.
“You guys have an excellent policy. And I believe you guys need to have that moral leadership to lead the rest of the world.”
That matters, because the only way to change the WHO is for countries like the UK to go to the WHO and tell them they need to change their position on vaping.
The end of what?
Clive Bates, Director - Counterfactual Consulting Ltd
By James
How to start? Clive’s presentation was so powerful I wanted to put every word in. Still, I’ll have a go:
The problem we have is not vaping - it’s smoking. As highlighted by other speakers too, that’s what’s killing millions - and killing them horribly.
What about the people who are going straight to vaping? Clive argues that the problem is solved for them.
“They will not be getting cancer, COPD, they will be vaping, they won't get sick, they'll probably be vaping in a transitory way.”
What about the ‘you shouldn’t vape if you haven’t smoked’ message?
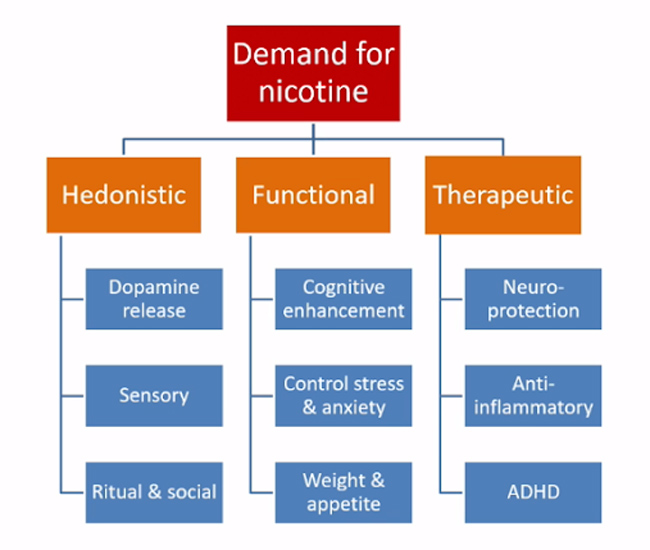
That’s like saying the only people who should take up drinking are the people who drink. The reality is that there will always be a demand for nicotine for hedonistic, functional and therapeutic reasons.
People stop using nicotine because it is bad for their health, but if that reason disappears we might realistically expect more use. In fact, maybe we should start to think of vaping as being more like caffeine or alcohol use.
What to do? The risk basis for policy should be combustion v. non-combustion, not tobacco v. non-tobacco.
What about false risk perceptions?
They decrease the focus on adult smokers, who are now not switching to vaping because they think it is more risky, and increase the focus on the flow of new nicotine users because it looks like these people are taking on a bigger risk. They also distort the entire debate around harm-reduction products.
Who’s to blame?
Understand there is a massive conflict of interest in harm. Without harm, there’s no tobacco control industry because there’s nothing to control, and no huge grants from organisations like Bloomberg. That’s why, in Clive’s opinion, some of the things that the tobacco control industry is doing are worse than what Big Tobacco did at the height of the 1970s:
“The extent of the deceit, the misdirection, the way that they're keeping people smoking is truly shocking.”
Closing Keynote: Keeping our eyes on the prize in nicotine and tobacco policy
Professor Robert West, Professor Emeritus of Health Psychology - University College London
By Kayleigh
Why are we here today, asks West? We're here:
“...because millions of people die unnecessarily, prematurely, and even more lives are ruined by chronic ill health because of tobacco use.”
He argues that our job is to discover how to reduce the death and disease of tobacco - and to do so in a way acceptable to policymakers and the public. While changing behaviour isn’t hard, it is difficult to do it in a way that is acceptable and affordable.
Society has become complacent about tobacco and we cannot become tobacco industry enablers. Prominent health organisations and public health experts have been spreading misinformation about vaping and, when e-cigarettes are presented as the new harm, this diverts attention from tobacco.
Biassed research, cherry-picked data and confusion of moral and health objectives on both sides of the debate leads to poor policy-making and public distrust - as seen with the Covid pandemic.
We are not in the smoking end game yet and we need to change our thinking. Health experts and policymakers need to move away from moralistic, black-and-white, elemental thinking to harm-focused, quantitative systems thinking.
Prof West emphasises the importance of this systems thinking - an approach that takes all factors into account and evolves the system over time. This approach will produce more helpful, non-black-and-white answers and lead to more evidence-based, harm-focused public health strategies.
Have your say
The summit is over for another year, but the issues aren’t.
Media-lead hysteria and misinformation have led to both calls for a crackdown on vaping and a UK consultation which includes options for vaping taxation, flavour restrictions and plain packaging. Evidence from speakers like Friedman suggests these measures will decrease (legal) vaping - but at the expense of increased smoking rates.
On the other hand, cigarettes are still causing huge amounts of disease and devastation, and an out of control vaping black market is likely to stymie attempts to curb vaping in favour of uncontrolled and potentially dangerous devices.
We also have some clear examples to look at. Thanks to vaping New Zealand is now at the ‘End Game’ with smoking, while draconian measures in Australia simply resulted in increased smoking rates, increased vaping rates and the utter domination of the black market.
Fortunately, you can have your say - the UK government consultation on vaping is open until the 6th December. Click here to share your response.